We have high standards in all we do.
Elite currently handles the accounts receivables and medical billing operations for Medical Billing companies, MSO and Anesthesia management companies.
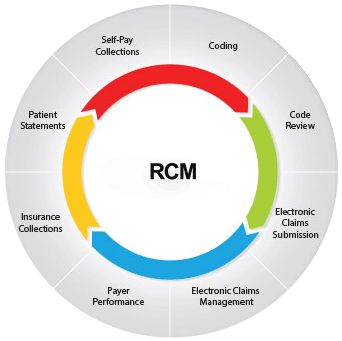
Elite offers comprehensive RCM solutions, with a wide range of business process services
Provider Credentialing and Enrollment – Documentation– Collect documentation and validate, Catalog and Store, Payer Submission- Identify top payers and file the application in payer-specific format, Ensure Enrollment- Timely follow-up of application and obtain the enrollment, Updates and Re-Credentialing-Periodic updates of the payer documents for recredentialling.
Eligibility & Benefits Verification and Prior Authorization – In the absence of proper eligibility and benefit verification, countless downstream problems are created – delayed payments, reworks, decreased patient satisfaction, increased errors, and nonpayment. Our team initiates prior authorization requests and obtain approval for the treatment through online portals and making calls to payers.
Demographics – Our accurate data processing ensures clean claims and does reduce denials drastically. Our experienced team registers all patient information with high accuracy. We ensure to choose the correct Insurance codes from the Insurance master list.
Medical Coding – Our AAPC and AHIMA-certified coders take care of specific Specialties and ICD-10 coding. They assist in documenting with appropriate CPT and ICD codes and Modifiers.
Charge Entry/Claim Submission – Our team has the ability to process both manual and review electronic charge entries available in EHR / EMR.
Payment/Denial Posting – The Payments received through ERA / EOB are posted on the system within 24 – 48 hours and the reports are reconciled on a daily basis. Denials are captured & moved to the Denial Analysis team.
Denial Management – Claim Denials are analyzed carefully, and the root cause is defined for each problem. It is then escalated to the concerned teams to make sure the Denials are fixed & also ensured they don’t recur in the future. Denial analysis is shared with the client once a week.
Accounts Receivables Follow-up – Elite’s objective is to improve your cash flow by reducing days in A/R and improving profitability by increasing your collections ratio. We analyze all underpayments and work with stakeholders to prevent them in the future.
We have expertise in all major specialities including
- Anesthesia
- Orthopedics
- Urology
- General physicians
- Diagnostic & Interventional Cardiology
- Gastroenterology
- Plastic, Reconstructive, and Aesthetic surgery
- Neurology
- Neurosurgery
- Endocrinology
- Primary Care Physicians
- Podiatry
- Psychiatry
- Radiology
- Other
The software we have experience with includes
- Advanced MD
- GE Centricity
- Avid Anesthesiology
- Med Evolve
- Clinical Works
- Medinformatix
- Allegiance MD
- Greenway Medical
- Medical Manager
- MISYS Tiger
- Helpers
- Kareo & MSI
- Office Ally
- Cerner
- Next Tech
Anesthesia Billing is Our strongest Specialty
At Elite, our primary expertise is in the anesthesiology billing process. We cater to hundreds of anesthesiologists and management companies in the U.S. We provide complete offshore outsourcing solutions for anesthesiologists. We understand how to appeal non-participating care contracts. We also understand how to handle the appeal of the non-paid cases, as well as how to constantly follow up on the denials. Our anesthesia collection rate is close to 98%
Virtual Assistance Services Include:
- Authorization management
- Referral management
- Credentialing using Pecos and CAQH
- AR follow up with insurance companies
- Text, chat, or phone support for your patients.
- Sending patient statements and analyzing accounts.
- Remotely assist your in-house staff with any non-clinical tasks.
- Financial reporting and custom reports development.
- Data entry of patient demographics.
- Data entry of patient charges
- Patient insurance eligibility verification.
- Charge review and approval.
- Claims submission to clearinghouse or medical payers.

